Plague: a widespread disease resulting in a high rate of death1
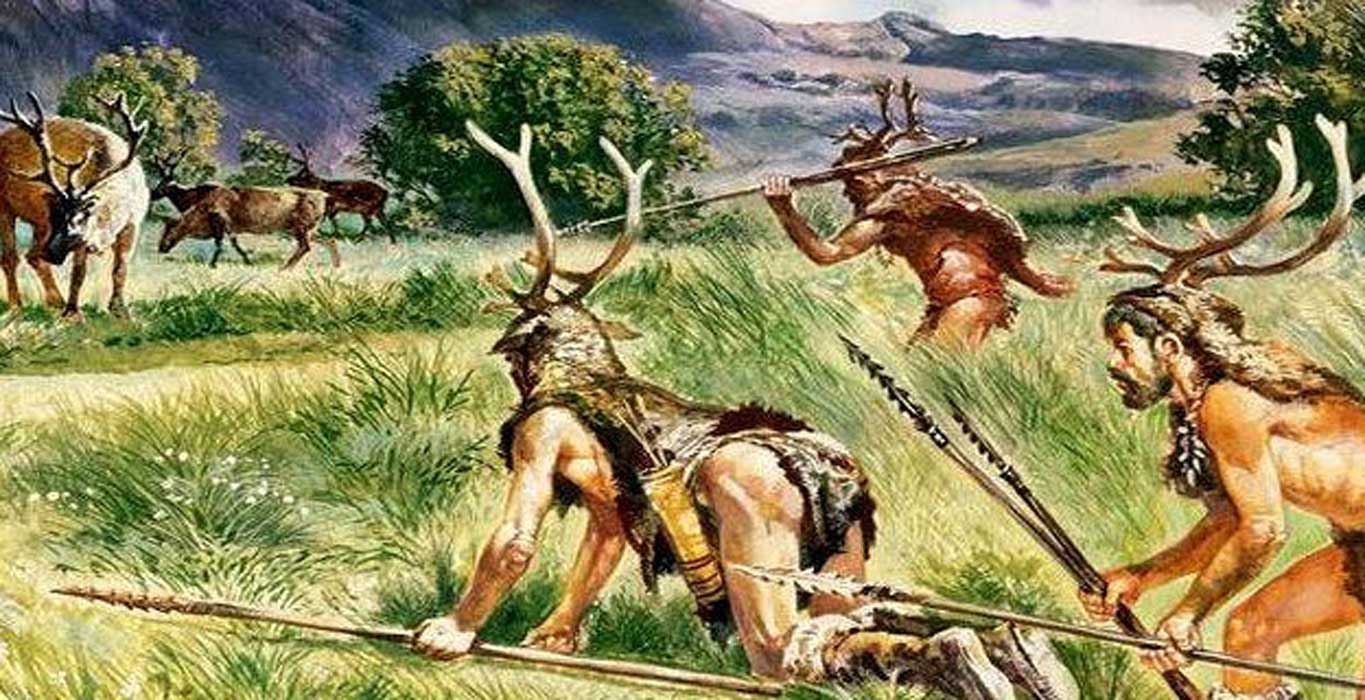
Before the time of established civilizations and booming societies, humans lived as hunter-gatherers roaming the land in small groups. The nomadic lifestyle of the time meant that there were fewer children (as they would have to be carried) and that groups were small, but it also meant that crowd diseases were non-existant and that there was limited exposure to rotted food and excrimants. Diseases that did ail these people included parasites, such as intestinal worms as well as lice and ticks, and illnesses associated with the microbes of the wild animals they encountered.2
As hunter-gathers abandoned this lifestyle and settled down, they began farming and domesticating animals. With this, the human population increased more than 100 fold.3 Crowd diseases became a real problem as well as vector bourne diseases from the animals raised in close quarters with humans. Food and water supplies were shared between human and animal, waste from both mixed and amassed, and insect, bird, and rodent vectors were attracted to human settlements, bringing with them new diseases and pathogens.4
Irrigation farming was one advancement that facilitated the growth of the population. Especially in drier, hotter environments, as it meant that food could be produced even during times when it would have been hard, or even impossible to grow food otherwise. However, with this innovation came ‘The Pharaoh’s Plague’ – also known as snail fever, or schistosomiasis. The shallow waters brought from rivers like the Nile and Euphrates flooded fields and brought with them disease causing schitosomes carried by aquatic snails.5
People of some ancient civilizations, like the Greeks and Romans, believed that cleanliness would appease their gods, not that it was beneficial for their health.6 Cleanliness, however, is a major contributor to limiting the spread of disease. In the 19th century, Dr. Semmelweis instituted the practice of handwashing amongst healthcare professionals when he noted a relationship between the rate of occurrence of perperal (childbed) fever among women in labor who were cared for by physicans with dirty hands, particularily those which just came from autospy.6
“In medical school, we were taught the ways people get sick, how they can be fixed, and rudimentary epidemiology of smoking, alcohol use, and unprotected sex. We were taught biology… Yet the theorectical knowledge regarding contributors to vast global inequities in health and suffereing is largely absent from medical school criteria.”7
Poverty is arguably the most prevelant factor for the cause and spread of disease. Studies have shown that there is a positive correlation between income inequality and infectious disease outbreaks. Census records of Chicago from the time of the 1918 Spanish Influenza epidemic show that in each area with a 10% increase in illiteracy- one indicator of poverty- that there was a 32% increase in flu-triggered death for that area.8 Areas of poverty and income inequality are a breeding ground for infectious diseases. The poor have neither the means nor the resources to change their conditions and seek the medical help that they need. They often live in cramped, crowded, sub-par conditions, and easily transmit disease not only amongst themselves, but across social classes as well. The poor cannot afford to miss work on unpaid sick leave, and are more likely to go to work while infectious- even if asymptomatic- and spread whatever is ailing them to others. Buildings with poor ventilation systems are the ideal habitat for Legionella, the pathogen responsible for the deadly Legionnaires disease.
“…diseases often lack attention when they first emerge because they affect the poorest populations of the world, meaning they are generally not profitable for pharmaceutical development.”9
Technology has also been a source for outbreaks in society. More than just with air conditioning units and ventilation systems, but also with products used by many in daily life. In the Unnited States alone, over 39 million women reported using tampons in 2018.10 A study conducted in 1998 found that 81% of participants and 71% of participating primary care physicians used tampons- either alone or in combination with pads. 92% of the physicians reported that their decision to or not to use tampons was influenced by their fear of toxic shock syndrome (TSS).11 This condition was first noted in 1978 in children and was associated with Staphylococcus areus, but was soon found to be more prominent among women that used tampons. The fiber technology used as an aid during a woman’s menstrual cycle trapped the bacteria within the vagina where it could flourish and produce toxins resulting in TSS.12 Technology has advanced to rectify this issue, but it is still always a risk to take into consideration when deciding to use this product.
“Many other aspects of globalization influence population health, including the accelerated emergence of new infectious diseaese, the near-ubiuitous rise in the rates of obesity and associated noncommunicable diseases as daily bodily energy budgets (food energy input vs. physical energy output) shift into surplus, the spread of cigarette marketing, the effects of climate change, increases in resistance in the workplace due to the deregulation of international markets.”13
The effect that the human population has on the world not only effects the way that we interact with the environment around us, but it also has lasting implications on the impact of the environment’s intercations with humans. Technological advances may improve many aspects of living, but have also polluted the earth with their emissions and greenhouse gases. Polluted air has been estimated to be the cause of roughly 6.5 million early deaths each year and pollution has led to climate change throughout the world.14 Climate change not only reshapes the environment, but it has had both positive and negative affects on human health. For example, warming, causing milder winters in more temperate areas could lead to fewer wintertime related deaths and hotter, drier conditions could reduce mosquito populations and thus mosquito-bourne infections.13 Conversely, it may lead to drought and an increase in wildfires that could further pollute the air and may result in the increase of respiratory disease.14
REFERENCES:
1https://www.merriam-webster.com/thesaurus/plague
2The Sedentary Lifestyle Power Point, Slides 9-10
3Ibid, Slide 13
4Ibid, Slide 23
5Ibid, Slide 37
6Chapter 11
7Lilic, N., et al. 2018. Murmurs of Politics and Economics. N ENGL J MED. 379(13):1202-1203.
8Moyer, M.W. 2018. Resurgent outbreaks of infectious diseases are sickening thousands and the causes are societal. Scientific American. May, p. 51.
9Parshley, L. 2018. Climate change is accelerating the spread of disease–and making it much harder to predict outbreaks. Scientific Americn. May, p. 62.
10https://www.statista.com/statistics/278085/us-households-usage-of-tampons/
11Omar, H.A., et al. 1998. Tampon use in young women. J Pediatr Adolesc Gynecol. 11(3):143-146.
12Chapter 1
13McMichael, A.J. 2013. Globalization, climate change, and human health.
14Haines, A. and Ebi, K. 2019. The imperative for climate action to protect health. N ENGL J MED. 380(3):263-273.